Abstract
Background:
Relapse after an allogeneic hematopoietic cell transplant (Allo-HCT) carries poor prognosis for patients with acute myeloid leukemia (AML). Central nervous system (CNS) relapse occurs at a relatively lower frequency among patients with AML (~5%) than with ALL (2-12%). CNS involvement by leukemia after Allo-HCT is often difficult to treat and no specific treatment algorithms currently exist. Very few studies examining the risk factors or management of CNS relapse exist. Further, prognosis for adult AML patients with isolated CNS relapse after Allo-HCT remains unclear. Due to the paucity of the data, we attempt to examine the leukemia relapse in CNS closely and characterize the incidence, risk factors and the effect on survival in our single institute retrospective study.
Methods:
We retrospectively reviewed all AML patients who underwent allo-HCT between 2006-2015 at Washington University in St Louis. We included patients aged >18 who underwent first Allo-HCT in complete remission. Isolated extramedullary relapse other than CNS, relapse after 2nd or more transplants, and transplants from cord blood were excluded. We included patients who had CNS only or bone marrow only as their first relapse. Isolated CNS relapse was defined as patients who had the first post-transplant relapse involving only CNS without evidence of relapse in BM. Patient's demographics, disease and transplantation characteristics were obtained in a retrospective manner. Kaplan-Meier method was used to plot survival outcomes and fine and gray approach was used to account for the competing risks.
Results:
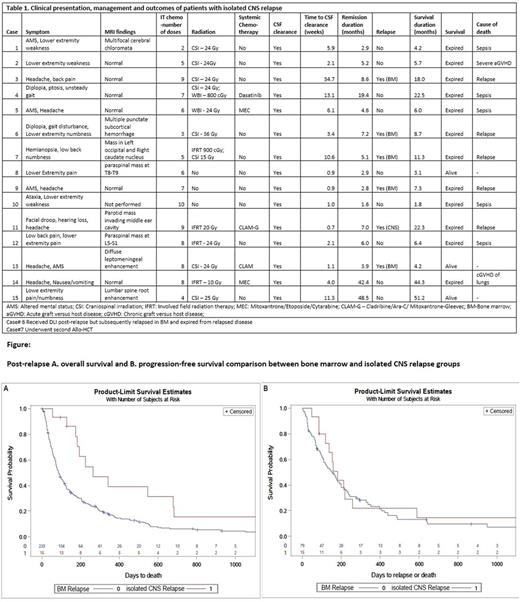
Of the total 940 patients that underwent allo-HCT between 2006-2015, a total of 249 patients had relapse after Allo-HCT (BM = 234 and isolated CNS = 15) and were included in the final analyses. Following pre-transplant and transplant characteristics were not statistically different between groups: age, HCT-CI, cytogenetic risk, type of transplant, stem cell source, conditioning regimen and immunosuppression. Median age is 56 years (18-74 years) in BM and 51 years (23-69 years) in isolated CNS group. More patients in BM group relapsed by day 100 post-allo. Median follow-up were 223 days and 85 days in isolated CNS and BM groups respectively. Median time to relapse was shorter in BM group (3.9 vs. 9.3 months; p=0.0017). All patients with isolated CNS relapse (15/15; 100%) achieved CSF clearance with intrathecal chemotherapy, systemic chemotherapy, or radiation (Table 1). After relapse, median time to CSF clearance was 3.4 weeks and median remission duration was 5.2 months. Five patients (33%) with isolated CNS relapsed in BM subsequently. In contrast, among patients with bone marrow relapse, seventy-nine (34%) achieved CR in with a median time to CR of 7 weeks. Post-relapse, median OS is longer in isolated CNS group compared to BM group (264 days vs. 87 days) with similar PFS. (Figure 1)
Conclusion:
We report very low incidence of isolated CNS relapse in AML patients who undergoing allo-HCT (1.6% in our study) in remission. Our study showed time from transplant to relapse was longer in isolated CNS relapse compared with BM relapse. These findings are consistent with previous studies that showed longer time to recurrence in extramedullary relapse than BM relapse. Outcomes of patients with isolated CNS relapse is poor despite high response rate to salvage therapy. Novel therapies are warranted to improve survival in post-allo relapses in general.
Uy: Boehringer Ingelheim: Consultancy; GlycoMimetics: Consultancy; Novartis: Consultancy, Other: Travel Suppport.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal